Osteochondrosis is a chronic disease of the spine. It develops with age and consists of degenerative-dystrophic changes that occur in the intervertebral discs. There were no symptoms for a long time. A person may notice only stiffness of the spine.
Osteochondrosis progresses slowly - many factors affect the speed of the disease. If the pathology is not treated, complications arise - sciatica, sciatica and others, depending on the spine. Some doctors believe that such a disease as osteochondrosis does not exist, and such a diagnosis is made only by those who do not understand human physiology.
Causes
In the 21st century, the disease, compared to the 20th century, has noticeably rejuvenated. Very often you can meet young people who have degenerative-dystrophic changes on the intervertebral discs during a medical examination for another pathology. There is only one reason for this - urbanization and progress.
Today, one does not have to struggle to get to work or to get food. Most lead a sedentary lifestyle, eat malnourished and quickly gain weight, walks in the fresh air and active activities prefer a computer and a comfortable sofa. Even before work, many get into their own cars, which are located in an underground garage on the territory of a multi-story building, and sit at their workplace for 7-9 or more hours.
Note. Osteochondrosis is only a human disease. None of the mammals had such a pathology. You have to understand that this is the retaliation of Homo sapiens for walking upright.
What causes osteochondrosis?
The following factors can promote the appearance of the disease against the background of physical inactivity, lack of sufficient physical activity and an unhealthy lifestyle:
- violation of mineral and vitamin metabolism;
- a large number of transmitted infectious diseases;
- chronic stress, depression;
- sudden movements, weight lifting;
- spinal injury;
- severe hypothermia;
- slouch
- curvature of the spine not noticed in time and not treated;
- long stay in an uncomfortable position (not necessarily sitting).
Note. Big sports have a negative impact on people's health. For example, lifting weights (and not only) in the future can become a trigger for degenerative-dystrophic changes in the intervertebral discs.
What happens to the spine?
The following factors directly affect back health:
- the blood circulation in the paravertebral tissues is disturbed, the intervertebral discs suffer from a lack of nutrients (they do not have their own blood vessels and depend on the tissues that surround them);
- the muscular corset that supports the spinal column weakens, the vertebrae receive an additional load that they cannot cope with;
- intervertebral discs lose moisture, decrease in volume and diameter - the spine seems to fall (many people notice that with age they become shorter by 5 or even 10 centimeters);
- there is instability of one or more parts of the spine;
- the body solves the problem of instability by growing osteophytes - these are marginal bony growths that over time firmly cement the spine, depriving it of flexibility.
Note. The transformation of the spine itself does not cause pain - the pain syndrome occurs when nerve roots, large arteries and lymphatic vessels are affected by osteophytes or the anatomical position of the vertebral body changes.
Symptoms
Signs of osteochondrosis increase as the disease progresses. There are 4 stages of pathology:
- First. Symptoms are completely absent. No pain. A person may feel a little more tired than usual, some stiffness of the spine, which he explains to himself as fatigue, excessive physical effort and overload. Osteochondrosis in the first stage can be
- A second. Persistent pain syndrome occurs due to injury to the nerve roots, which is easily stopped with non-steroidal anti-inflammatory drugs. If the patient continues to ignore his body's signals and does not go to the doctor, the disease progresses rapidly. The flexibility of the spine decreases, especially in the cervical and lumbar areas. The appearance of the vertebral artery syndrome is probably caused by its compression or edematous paravertebral tissue or a displaced vertebra.
- Third. Pathology in a neglected state. The pain haunts a person for 24 hours, slightly weakens in a horizontal position, but it is impossible to stay in one position for a long time (on the back, on the side). Sleep is disturbed, the patient becomes irritable. A person bends down (chest, lumbar) trying to find a more comfortable position that would not cause discomfort, which becomes an incentive for humps, scoliosis and other deformities of the spine.
- Fourth. Accumulation of osteophytes occurs - stabilization of the spine. The patient can look around only by turning the trunk completely. The pain is strong, constant, completely removed only by blockades (novocaine, prednisolone). Disability in the fourth stage is about 80%.

Simultaneously with the mentioned signs, the patient may suffer from symptoms that at first glance have nothing to do with the back - dizziness, flies in the eyes, arterial hypertension, numbness of the upper extremities (cervical osteochondrosis), chest pain that mimics an angina attack or cardiac, intercostal neuralgia (thoracic osteochondrosis), cauda equina syndrome, numbness of the lower extremities (lumbosacral osteochondrosis).
Note. Pathology causes vegetovascular and neurodystrophic disorders.
Diagnostics
To establish an accurate diagnosis, the patient is sent for an X-ray, myelography and neurological examination of reflexes. If that is not enough, the referral is issued to:
- MRI (magnetic resonance imaging);
- CT (computed tomography);
- NMR (nuclear magnetic resonance).
The doctor also interviews the patient and performs a medical examination, which reveals painful areas, possible curvature of the spine, leg length difference and other objective signs of spinal damage.

Therapy
Treatment of osteochondrosis is complex. To stop the degeneration process, or at least slow it down, they are assigned:
- chondroprotectors - externally, orally (oral), in injections to restore cartilage tissue;
- muscle relaxants - relax spasmodic muscle groups, used only under medical supervision;
- pain relievers;
- blockades - relieve pain for a long time, but do not cure;
- physiotherapy (magnetotherapy, phonophoresis, vibration therapy, EHF, etc. );
- exercise and original gymnastics;
- massage;
- acupuncture;
- balneo and mud therapy.
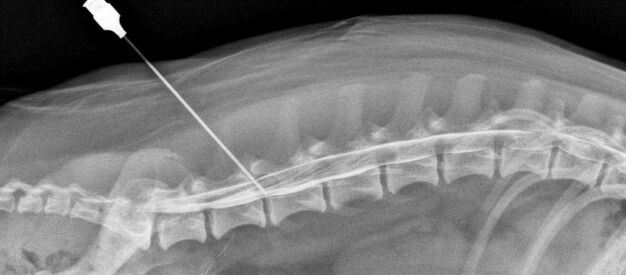
In advanced cases (uncontrollable urination and defecation, cauda equina syndrome), surgical intervention may be required to decompress and stabilize the affected spinal segments.
Decompression operations with a posterior approach:
- facetectomy;
- foraminotomy;
- laminectomy;
- laminotomy.
Decompression operations with an anterior approach:
- discectomy;
- corpectomy.
Spinal fusion is used to stabilize the damaged segment - the fusion of adjacent vertebrae using a special fixed structure (spines). A bone implant is placed in place of the removed intervertebral disc (bone material is either taken from a donor or formed from the patient's own bone).

Note. Spinal fusion can be avoided. Surgeons have achieved a lot in the surgical treatment of osteochondrosis. Instead of the removed intervertebral disc, it is possible to implant an artificial one and thus avoid complete immobilization of the segment. Spine operations are full of many complications, so they are prescribed only in extreme cases.
Prevention
Even Hippocrates said: "It is easier to prevent a disease than to cure it. "This rule also applies to osteochondrosis. It is enough for a person to monitor his health, lead an active lifestyle, eat properly, exercise regularly in order to maintain the health of the spine.

If the disease does manifest itself, prevention will help prevent it from starting. Follow these guidelines:
- Sleep on the right mattress and pillow. Choose an orthopedist and consult your doctor first.
- Make it a rule to walk for at least half an hour before and after work. During the break, don't sit at the computer or the phone, but warm up and then have a snack.
- Watch your weight. The bigger it is, the harder it is on the spine.
- Adhere to the rest regime (work during the day, sleep at night).
- Try to eliminate stress from your life. If you feel that you are falling into depression, see a specialist.
Note. Traditional healers claim that osteochondrosis can be cured with the help of medicinal plants. It is difficult to say how true this statement is. Treatment with alternative methods can be used in addition to the one prescribed by the doctor. Otherwise, the result is not guaranteed.
Osteochondrosis is a dangerous disease, fraught with disability if treatment is not started on time. If you feel that you tire suspiciously quickly, and in the morning your spine is less flexible than before, consult a doctor and undergo a complete examination. In the initial stages, the pathology can slow down and even stop completely.

























